CHSP's March 2024 Topic: Invisible Diseases
Invisible Illnesses have symptoms others can't point out just by looking at someone. "There's no strict medical definition, but invisible illnesses are diseases that affect a person's ability to conduct their lives as they'd like to but that you can't 'see."
An April 2021 Disability & Society study indicated that "there are perceptions that chronic illness is not a valid disability due to its invisibility." This may in part be because many invisible illnesses cannot be diagnosed by a simple blood test or tissue biopsy. And many have subjective symptoms, like fatigue, headaches, and body pain, that could be associated with hundreds of different medical conditions.
Some of these conditions do not show visible signs until they are more advanced or some diseases affect people differently. For example, everyone with MS is different so there are going to be people who have visible signs of MS from the time of diagnosis versus others who won't. Every person, every case can be different.
The following are just examples of Invisible Illnesses:
| ADHD | Anxiety Disorders | Allergies |
| Arachnoiditis | Asperger Syndrome | Asthma |
| Autism | Bipolar disorder | Brain injuries |
| Charcot Marie Tooth disease | Chronic Fatigue Syndrome | Chronic Pain |
| Circadian rhythm sleep disorders | Coeliac Disease | Crohn's disease |
| Depression | Diabetes | Ehlers Danlos Syndrome |
| Endometriosis | Epilepsy | Fibromyalgia |
| Food allergies | Fructose malabsorption | Hereditary Fructose Intolerance |
| Hyperhidrosis | Hypoglycemia | Inflammatory bowel disease |
| Interstitial cystitis | Irritable Bowel Syndrome | Lactose Intolerance |
| Lupus | Lyme Disease | Major depression |
| Metabolic syndrome | Migraines | Multiple Sclerosis |
| Multiple Chemical Sensitivity | Myasthenia Gravis | Narcolepsy |
| Personality disorders | Primary immunodeficiency | Psychiatric disabilities |
| Reflex Sympathetic Dystrophy | Repetitive stress injuries | Rheumatoid arthritis |
| Schnitzler's Syndrome | Schizophrenia | Scleroderma |
| Sjogren’s syndrome | Temporomandibular joint disorder | Transverse Myelitis |
| Ulcerative Colitis |
Results:
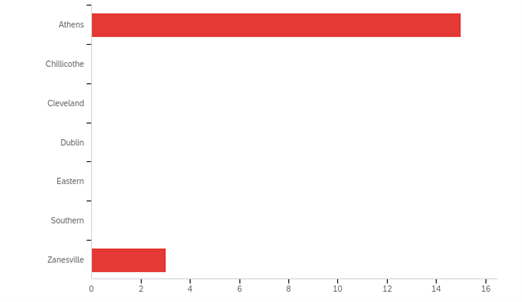
At which Campus do you currently attend/work?
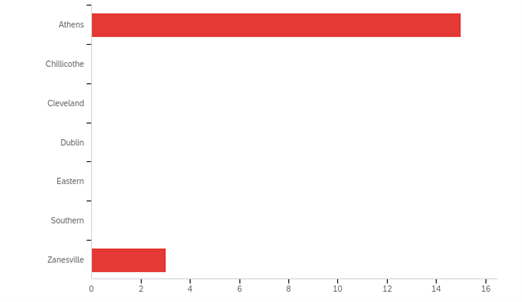
*A total of 18 responses were received. 15 were from Athens Campus and 3 were from Zanesville Campus.
You are currently a:
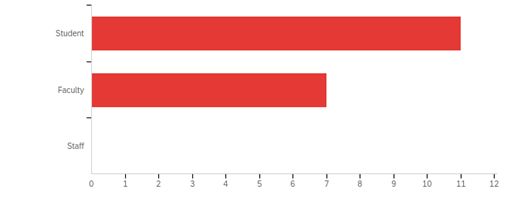
*Results were 11 students and 8 faculty members completed the survey.
Have you heard the terms Invisible Disability, Illness, Invisible Diseases, or Invisible Disorders?
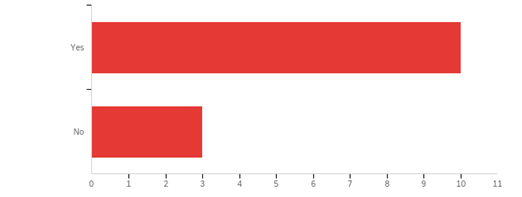
*Results were 13 people had heard of invisible disabilities and 3 people had not heard the term.
Do you, or someone you know, have an invisible disability, illness, disease or disorder?

*Results were 13 people said they or someone they know have an invisible illness or disability.
As a future, or present, healthcare provider, do you believe you know enough about invisible diseases?
- No, there are so many and some are so rare, it is difficult to know enough.
- I can always learn more.
- No
- Yes, but I do still think there is a stigma around illnesses/diseases that cannot be seen. I think those who suffer from these usually go through hoops to get providers to believe them.
- I don’t believe that I do. More often than not these invisible disabilities aren’t discussed and given the same ‘respect’ in the healthcare field. Even though they may not be easy to see from the surface doesn’t mean that they are not prevalent and a major component of many people’s lives.
- I can always know more!
- I know about invisible diseases but I can and should always learn more!
Invisible disabilities are the most common type of disability among college students. With this knowledge, what methods would you use to successfully work with others who may have an invisible disability?
- First of all, if you know they have an invisible disability, believe them. Ask them what you could do to make whatever it is you are doing with them, easier. If you are providing care, ask about the symptoms and what makes the symptoms better or worse. Ask them if they notice any correlation between symptoms and other factors in their life (light, noise, stress, exercise, etc.).
- I think asking questions is the key. I think providers need to be empathetic and listen more. We live in a world that revolves around billing hours and how many patients can be seen in a day. I think a lot of people could get diagnosed earlier if providers listened more. I have been ignored by nurses, doctors, and other healthcare providers in the past and I know how that can make an individual feel.
- Since invisible disabilities are so prevalent with college students it’s really important to create a space/environment where they feel comfortable discussing their lives and issues. More than anything else young adults care about appearances. This can cause a lot of loneliness and puts a heavy burden on these individuals to be ‘perfect’. Groups and clubs promoting this inclusivity and excellence are crucial.
- I try to welcome students to share as much or as little with me as they are comfortable, I welcome and encourage accommodations, I am flexible in the classroom and ask students what they may to be successful that I can help support them.
- Continue to reach out to students who are absent or struggling to build relationships so I can better determine underlying causes that can be managed in a collaborative way.
